TRANS-
FORMATIVE
Technologies
TRANS-
FORMATIVE
Technologies
Transformation. Unlocked.
DynamX® Drug Eluting Coronary Bioadaptor System
A significant innovation in the treatment of coronary artery disease, DynamX represents one of the most significant breakthroughs in coronary implant design in the past 30 years. The future of vascular intervention won’t just evolve, it will adapt.
Restore
Intervene, don’t interfere.
First step in any intervention is restoring blood flow. And, with DynamX you may achieve significant acute lumen gain without compromising the ability for the vessel to naturally heal.
Release
Unlock the rush of freedom.
After 6 months the magic happens. DynamX unlocks itself, releasing the vessel to pulsate more freely, respond to every heartbeat, increasing vital blood flow.
Return
Arrive at a more natural state.
Finally, the vessel returns back to its natural physiology, motion and function. It’s free to adapt and maintain optimal lumen size while DynamX continues to provide dynamic support.
The Dynamx bioadaptor scaffold is comprised of three metallic helical strands that are linked together by unique unlocking elements. The helical strands separate following natural resorption of the biodegradable polymer coating, allowing for restoration of vessel motion and function.
BIOADAPTOR RCT
In a large, randomized, controlled trial comparing the bioadaptor to a leading drug eluting stent (DES), DynamX demonstrated superiority across key endpoints such as in-device pulsatility and significantly lower late lumen loss, reflecting the unique value of increasing blood flow and allowing for positive adaptive remodeling.
*The DynamX bioadaptor is CE marked. Not approved in the US.
International (OUS) Use Only. DynamX is intended to improve coronary luminal diameter in patients with symptomatic ischemic heart disease due to discrete de novo native coronary artery lesions. CAUTION: The law restricts this device to sale by or on the order of a physician, indications, contraindications, warnings and instructions for use can be found in the product labeling supplied with each device.
Potency where it’s needed most
Site-Specific Antithrombotic Therapy (TRx)
TRx is the world’s first triple-drug site-specific antithrombotic therapy using two anticoagulants (rivaroxaban and argatroban) and an antiproliferative mTOR inhibitor, sirolimus. The therapy is designed to address challenges associated with percutaneous coronary intervention (PCI), including management of ischemic and bleeding risk due to use of systemic oral antithrombotic medications.
Harnessing the power of many
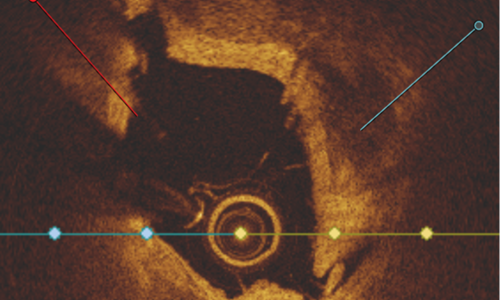
Intravascular Hertz Contact Lithotripsy
Leveraging the power of physics and mechanics, our Intravascular Hertz Contact Lithotripsy Catheter is designed to effectively fragment calcium without the need for capital equipment or disrupting standard PCI procedure workflow.
Using multiple discrete stress points to fracture calcium the system is designed to effectively treat concentric and eccentric calcified lesions.
PMN 1709 Rev A
